What is hemodialysis?
Hemodialysis is a medical treatment for patients with kidney dysfunction to filter waste and water from the blood. This procedure helps stabilize patients’ blood pressure and balance various electrolytes in the blood.
Outpatient hemodialysis centers located in different communities throughout Los Angeles County are critical to ensuring that all patients in need of dialysis have access to this important medical procedure. Here you will find information, resources, and updates for both patients and healthcare workers connected to this setting.
Infection Control in the Dialysis Setting
Hand hygiene is the most vital step in infection prevention in all settings, especially in outpatient hemodialysis facilities. Hand hygiene must be performed:
- Before touching a patient
- Prior to performing an aseptic task (e.g., placing an indwelling device) or handling invasive medical devices
- Before moving from a contaminated body site to a clean body site on the same patient
- Following a procedure involving exposure risk to body fluids
- After patient contact and glove removal
- After contact with patient surroundings including touching any object, furniture, or patient belongings

There are two different methods of hand hygiene that can be performed
Alcohol-based hand rub (ABHR):

- Recognized as the most effective products for reducing germs on the hands of healthcare providers.
- Preferred method for routine patient care.
- Cover all hand and wrist surfaces and rub until completely dry.
- Drying typically takes ~15–20 seconds.
Soap and Water
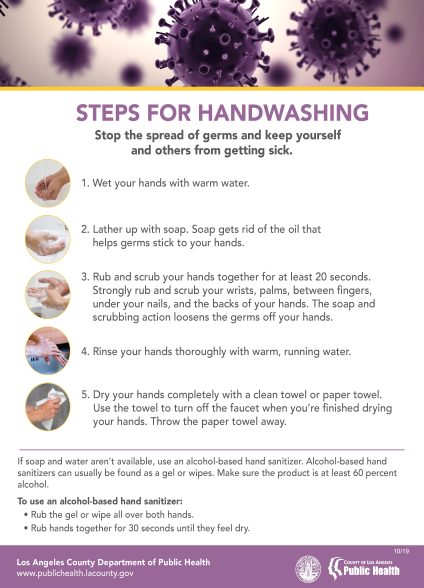
- Use when hands are visibly dirty, before eating, and after using the restroom.
- Rub for about 20 seconds, covering all hand and wrist surfaces.
- Required after caring for patients with C. diff.
See more hand hygiene materials here.
Observing disinfectant contact/wet times ensures skin is properly disinfected prior to cannulation and decannulation. Train staff on your facility’s specific products before use.
Common active ingredients:
- Alcohol
- Chlorhexidine
- Iodine
- Sodium hypochlorite skin solutions
Not all products are the same. Follow manufacturer instructions for use (IFUs) consistently.
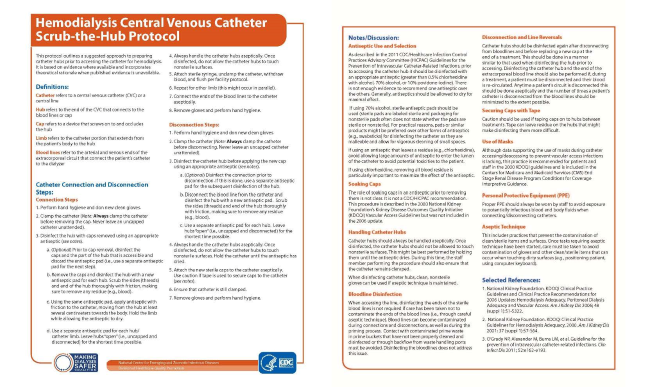
CVCs may be required for access and carry the highest infection risk among access types.
The CDC Hemodialysis Central Venous Catheter “Scrub the Hub” Protocol provides guidance on connection, disinfection, and maintenance.
IV/injectable meds are common; safe injection and proper prep are essential.
Medication Preparation
- Begin with proper hand hygiene
- Use a designated, clean prep area away from patients
Injectable and Intravenous Medications
- New syringe and needle each entry
- Scrub vial septum with alcohol before entry
- Multi-dose vials can be accessed aseptically more than once; single-dose should not
- Prepare close to administration time; avoid predrawing
- Never leave a needle in a vial septum
Medication Administration
Follow infection control protocol. See CDPH Injection Safety Information.

Station disinfection issues include improper storage, wrong products, insufficient use, and incorrect sequence.
Recommendations include:
-
Disinfectant Type and Storage
- Use an EPA-approved disinfectant for the setting/organisms
- Follow IFUs for storage
- Dilute correctly (e.g., 1:10 or 1:100 bleach as indicated)
- Store diluted solutions covered; keep away from sinks unless a barrier prevents contamination
-
Disinfection Process
- Wipes must be saturated enough to meet contact/wet time per IFUs
- Clean top-down; avoid recontaminating cleaned items
-
For Administrators
- Provide training and refreshers when products/processes change
Use internal audits and annual skills training to ensure policy compliance and identify improvement areas.
See CDC/NHSN quality tools: Audit Tools and Checklists | Dialysis Safety | CDC
Train staff on new equipment, supplies, or procedures before implementation.
Follow infection control guidelines for safe water use. See CDC: Water Use in Dialysis.
Clear, timely communication—especially of colonization/infection status—prevents spread to other facilities. Resources: LAC DPH Interfacility Transfer Resources
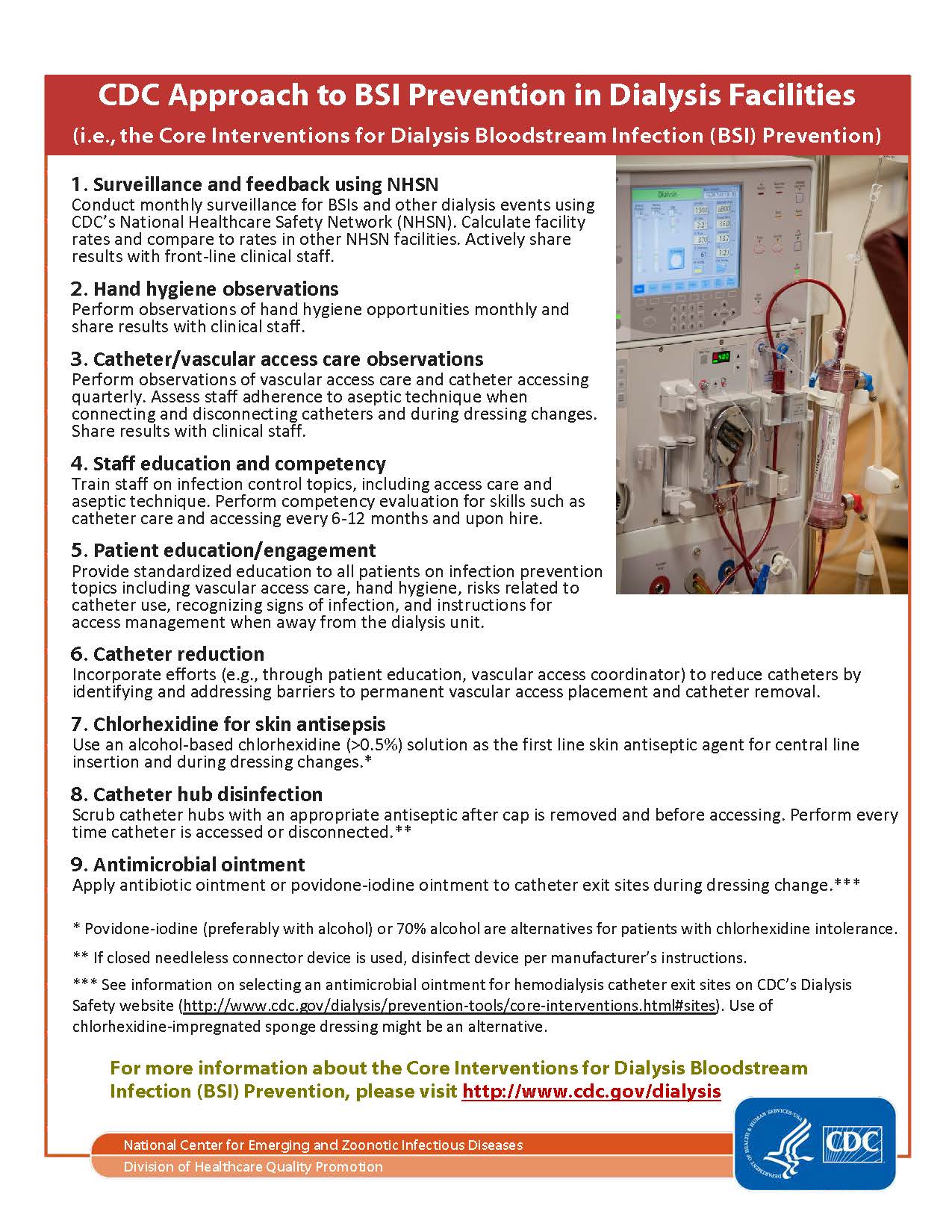
These interventions form the foundation of the CDC’s Dialysis BSI Prevention Collaborative, which has been shown to significantly reduce bloodstream infections in outpatient hemodialysis facilities.
- Surveillance and feedback using NHSN monthly surveillance for BSIs, actively share results with staff
- Perform observations of hand hygiene opportunities monthly and share results with clinical staff.
- Perform observations of vascular access care and catheter accessing quarterly, actively share results with staff.
- Train staff on infection control topics, perform competency evaluation for skills every 6-12 months and upon hire.
- Provide standardized education to all patients on infection prevention topics.
- Incorporate efforts to reduce catheters by switching to permanent vascular access placement and catheter removal
- Use an alcohol-based chlorhexidine (>0.5%) solution as the first line skin antiseptic agent for central line insertion and during dressing changes (Povidone-iodine (preferably with alcohol) or 70% alcohol are alternatives for patients with chlorhexidine intolerance)
- Scrub catheter hubs with an appropriate antiseptic after cap is removed and before accessing. Perform every time catheter is accessed or disconnected.
- Apply antibiotic ointment or povidone-iodine ointment to catheter exit sites during dressing change
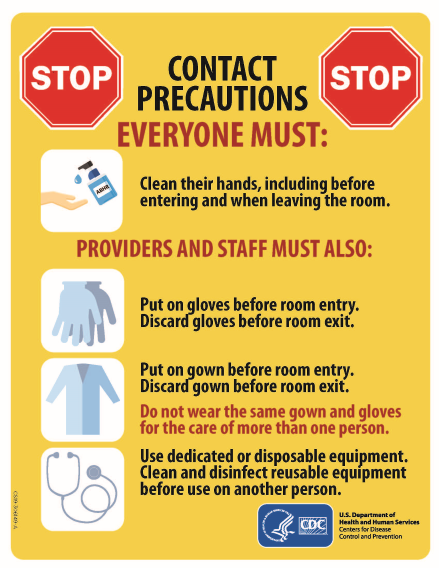
Isolation Precautions in the Dialysis Setting
Like all other healthcare settings, outpatient dialysis facilities must face the challenge of preventing infectious disease transmission and implementing appropriate isolation precautions in order to protect their patients. Below are some topics of concern that are relevant to the outpatient dialysis setting.
Isolation Rooms
- Outpatient dialysis facilities built after 2009 are required to have isolation rooms for the treatment of hepatitis B virus positive (HBV+) patients unless they are granted a waiver, per CMS requirements.
Equipment
- Equipment used for the care of HBV+ patients must be separate and dedicated to this patient population. They must not be routinely removed from the isolation room/area.
Staff
- Staff must use separate gowns when providing care for HBV+ patients and discard gowns before leaving the isolation area/room.
- Staff providing care for hepatitis B surface antigen (HBs-Ag) positive patients should not be caring for HBs-susceptible patients at the same time, in the same shift, or during patient changeover.
- Staff must ensure proper adherence to hand hygiene measures and change gloves frequently.
In general, additional contact precautions are not recommended in hemodialysis units for patients infected or colonized with pathogenic bacteria for several reasons, including difficulty determining transmission sources and reduced transmission time compared with acute care. Routine practices in dialysis are already more stringent than Standard Precautions.
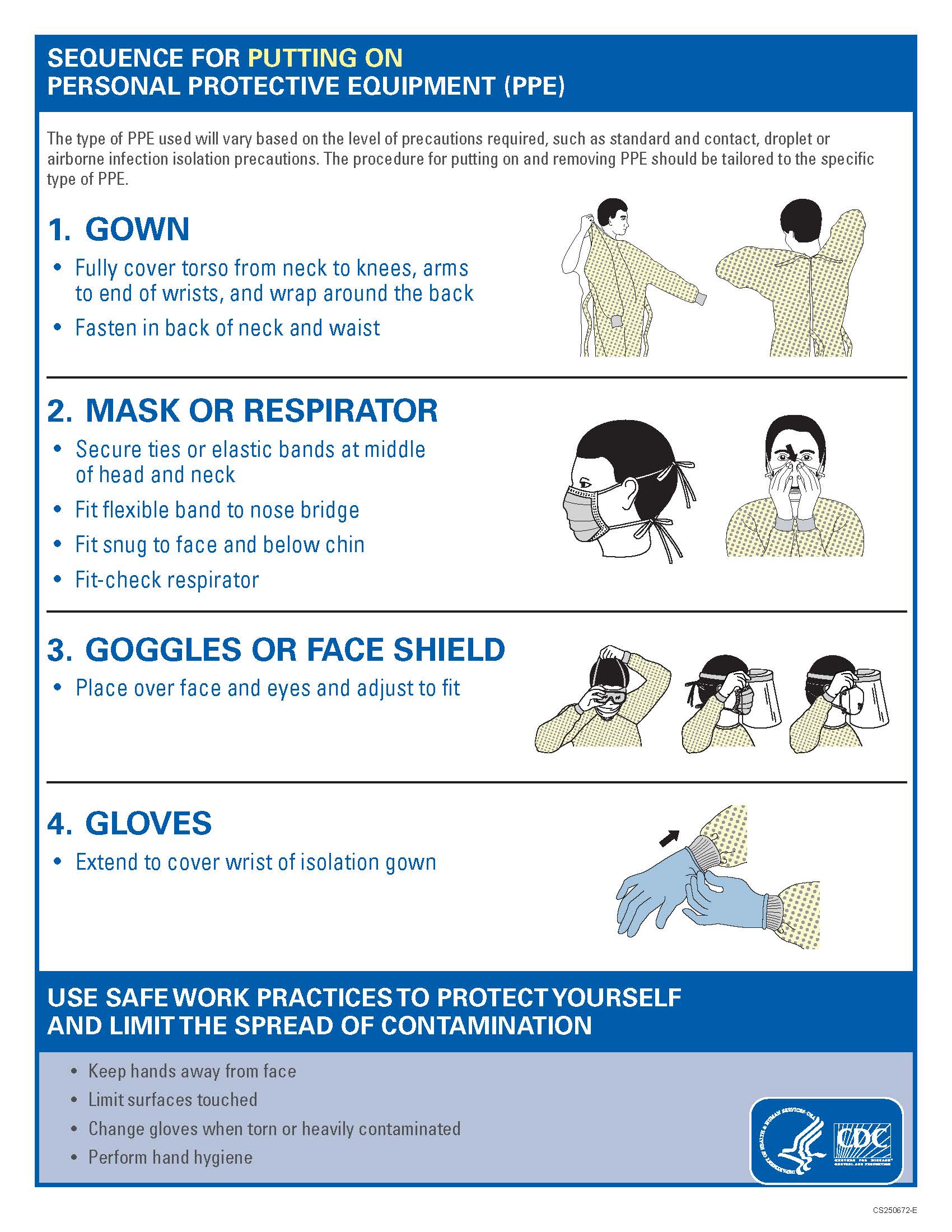
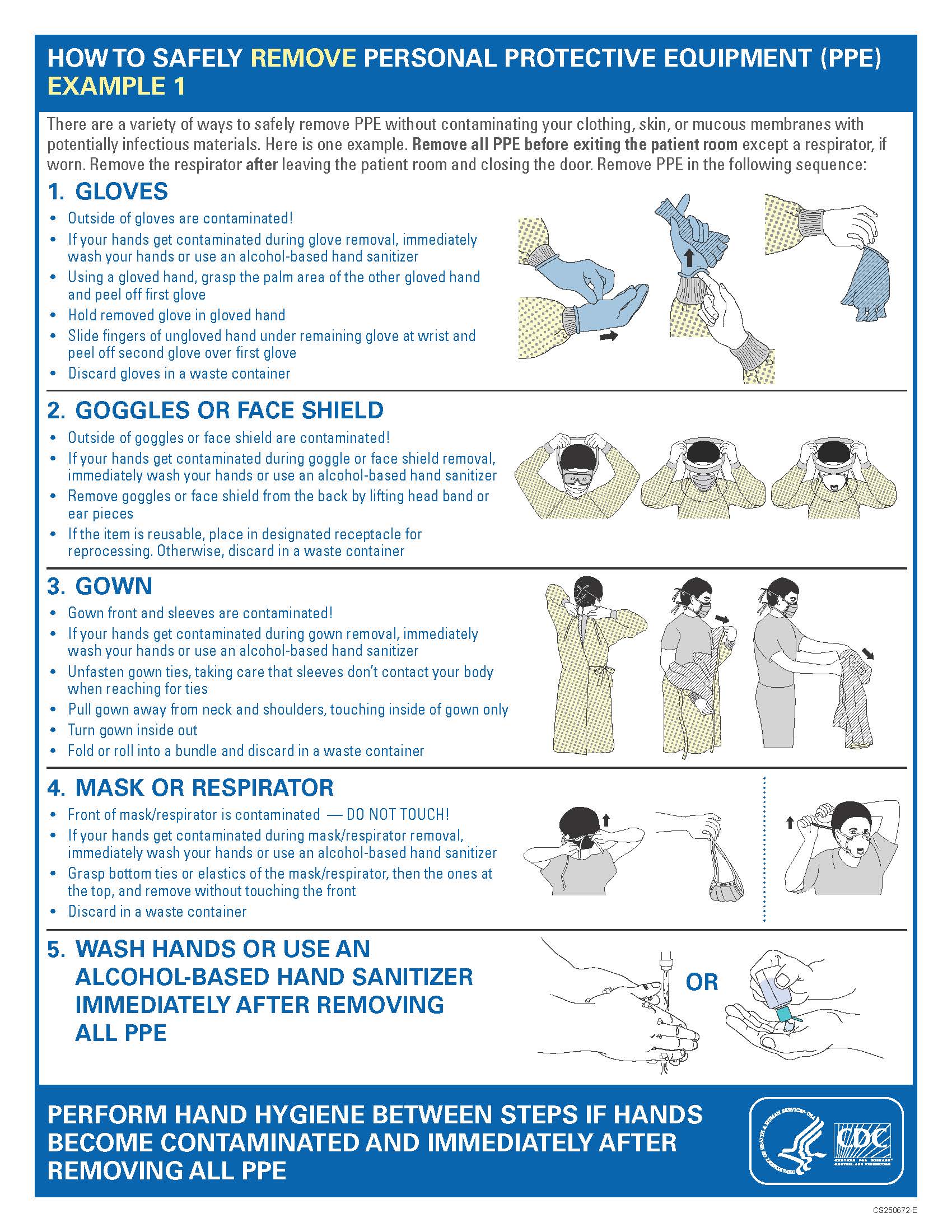
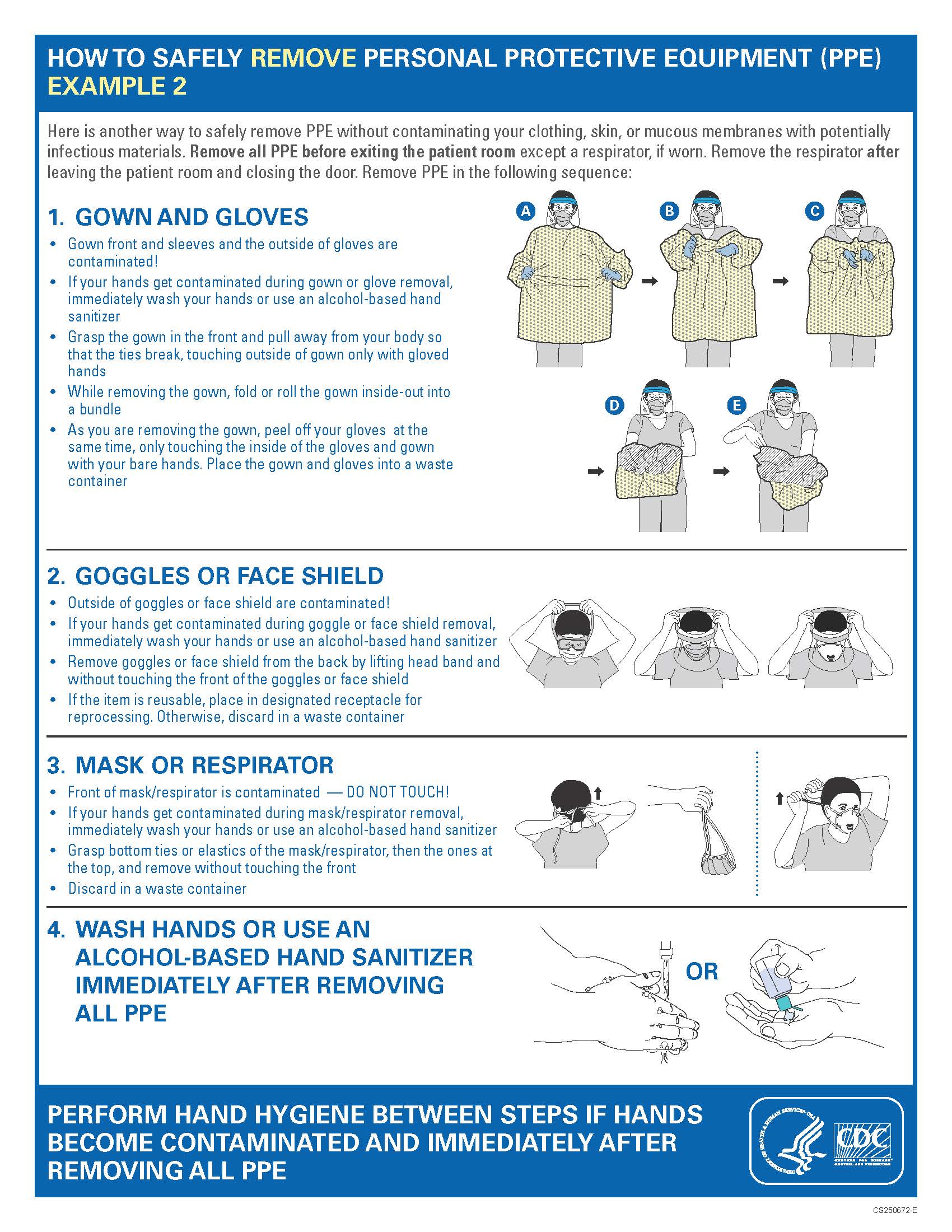
Strict adherence to hand hygiene, PPE, and environmental cleaning is critical. Facilities may consider additional measures based on resources, including patient cohorting.
LAC DPH has created a C. auris FAQ for dialysis centers:
Patient FAQ
Infections are prevalent among dialysis patients and can be serious. Germs spread through person-to-person contact, respiratory droplets, contaminated surfaces/equipment, or unwashed hands.
A bloodstream infection (BSI) is serious and most often linked to central line catheters. Symptoms include:
- Fever
- Chills
- Low blood pressure
Viral infections are also a concern and can spread through contaminated blood or surfaces. Examples include:
- Hepatitis B
- Hepatitis C
- HIV
Risk of Infections for Vein Access Types
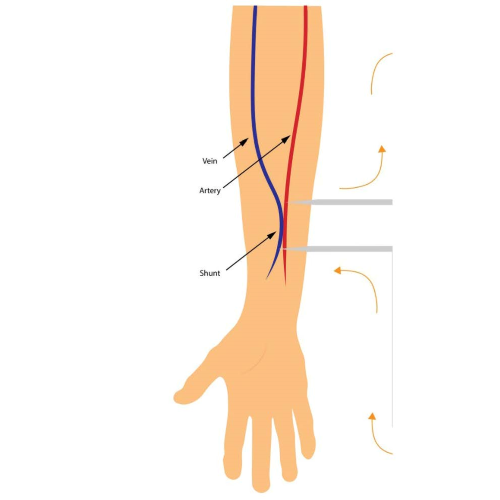
Arteriovenous (AV) Fistula
Created by connecting an artery and vein, usually in the arm. Long-lasting and the lowest infection risk.
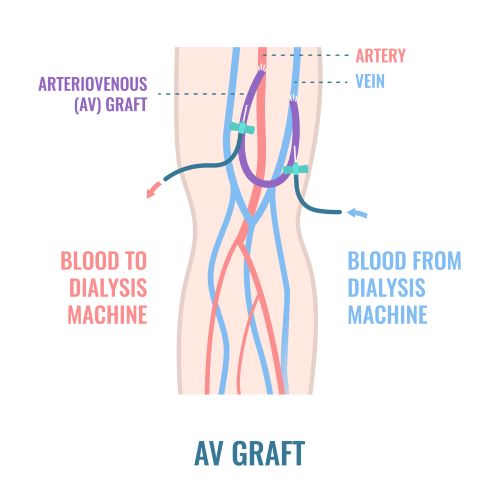
Arteriovenous (AV) Graft
Uses a tube to connect a vein and artery. Higher infection risk than a fistula but lower than a catheter.
Central Venous Catheter (CVC)
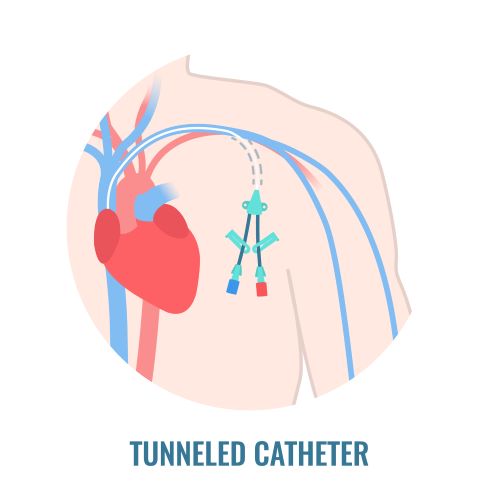
Inserted into a large vein in the neck, chest, or groin. Highest infection risk among access types.
Signs of infection include:
- Fever
- Swelling, redness, pain, or drainage at the access site
Patients can help prevent infections. The CDC recommends:
- Wash hands regularly or use alcohol-based hand sanitizer.
- Cover your nose and mouth when you cough or sneeze.
- Learn what to expect during dialysis and how staff keep you safe.
- Check your access site daily and tell staff if you see redness, drainage, or swelling.
- Tell staff if your catheter dressing becomes dirty or wet.
- Ask if a fistula or graft is possible if you have a CVC.
Educational Resources/Training
Previous Presentations:
- Candida auris: Best Practices in Dialysis Settings (07/30/2021) slides
LAC DPH Dialysis Team Highlights
2022 Infection Control and Response Project
In 2022, LAC DPH conducted an Infection Control and Response (ICAR) project in an effort to decrease outpatient dialysis BSI rates in Los Angeles County. LA County has 176 hemodialysis outpatient facilities and, prior to this project, had not had a large-scale collaboration project with these facilities. The Outpatient team conducted ICAR visits in 22 outpatient dialysis centers focusing on BSI prevention process measures. ICARs consisted of on-site infection control observations, completion of the CDC Infection Control Assessment Tools, and providing education and recommendations. Afterward, the team provided a resource binder and an email follow-up including a summary of observations conducted and recommendations to improve infection control practices for each dialysis center. The ICARs have fostered relationships with Los Angeles County hemodialysis centers that were previously unexplored.